 Finding innovative, minimally invasive ways to treat liver cancer”and being able to tailor that treatment individually to patients”are hallmarks of interventional radiologists. Advances in yttrium-90 (Y-90) radioembolization for liver cancer, a leading cause of cancer deaths worldwide, are reported in studies in the October Journal of Vascular and Interventional Radiology.
Finding innovative, minimally invasive ways to treat liver cancer”and being able to tailor that treatment individually to patients”are hallmarks of interventional radiologists. Advances in yttrium-90 (Y-90) radioembolization for liver cancer, a leading cause of cancer deaths worldwide, are reported in studies in the October Journal of Vascular and Interventional Radiology.
“Results of these two new studies may be beneficial to patients with liver tumors that cannot be surgically removed,” said Daniel Sze, M.D., Ph.D., FSIR, professor of interventional radiology at Stanford University Medical Center, Stanford, Calif. “These studies address methods to modify the blood vessels of the liver in order to maximize delivery of tumor-killing material to the targets and to make treatment simpler and safer,” he added.

“Blood supply to tumors can be complex and can present challenges for interventional radiologists,” said Riad Salem, M.D., MBA, FSIR, who wrote an accompanying commentary in JVIR. “This research advances the field and provides information that is immediately applicable to all interventional radiologists when treating their cancer patients,” said Salem, professor of radiology, medicine and surgery and director of interventional oncology, division of interventional radiology, in the department of radiology at Northwestern University in Chicago, Ill. “Such research allows interventional radiologists to tailor treatments to help even the sickest patients achieve a better quality of life,” he explained.
Worldwide, primary liver cancer accounts for an estimated 600,000 deaths annually. Last year, it was estimated that 24,120 new cases of primary liver cancer and intrahepatic (within the liver) bile duct cancer would be diagnosed and 18,910 people would die of these cancers in the United States. Primary liver cancer shows the most rapidly increasing incidence of all cancers in this country. In addition, roughly ten times as many patients succumb to liver cancers that spread from other sites.
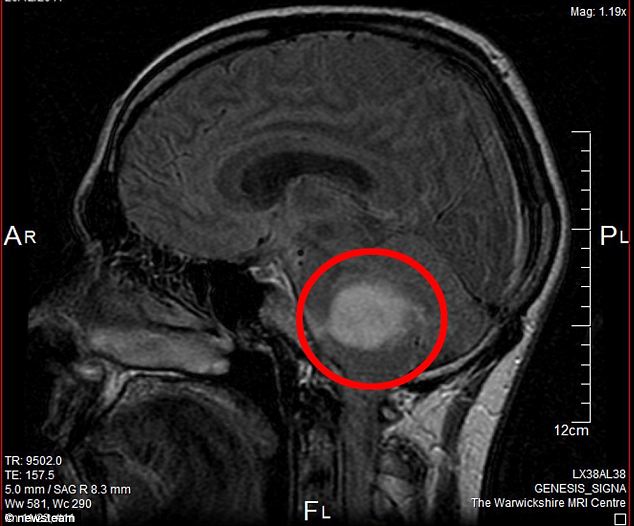
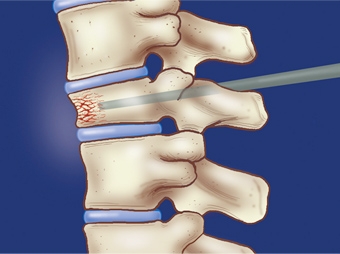
Many of these patients may be treated with Y-90 radioembolization. With Y-90 radioembolization treatment, radioactive microspheres (tiny beads) are injected through a catheter from the groin into the liver artery supplying the tumor. The beads become lodged within the tumor vessels, where they emit radiation locally that causes tumor cells to die. This technique allows for a very high local dose of radiation to be delivered, with little danger from radiation to the healthy tissues in the body, said Salem.
While radioembolization is palliative”not curative”the treatment benefits patients by extending lives and by improving symptoms and is associated with fewer side effects than traditional treatments for cancer. Interventional radiologists have long studied the use of intra-arterial (delivery of treatment via an artery) therapies for cancer and pioneered yttrium-90 radioembolization since its introduction in 2000 to treat liver cancer.
One study showed promising results in a group of 35 patients in whom the “thirsty tumors” had recruited blood vessels from outside the liver, a situation that interferes with complete delivery of Y-90 microspheres to the tumors, explained Sze. “These ‘parasitized’ blood vessels were successfully embolized, or closed off, before administration of Y-90 microspheres, reestablishing the blood supply from within the liver to enable the successful delivery of the microspheres to the targeted tumors,” said Sze, senior author of “Embolization of Parasitized Extrahepatic Arteries to Reestablish Intrahepatic Arterial Supply to Tumors Before Yttrium-90 Radioembolization.”
“While large, multicenter studies will be necessary to further confirm the proof of the concept, it is notable because the Stanford University researchers investigated the idea of simplifying blood supply in order to permit a direct injection of microspheres into the tumor,” said Salem.
In a related report, “Consolidation of Hepatic Arterial Inflow by Embolization of Variant Hepatic Arteries in Preparation for Yttrium-90 Radioembolization,” the same team was able to make treatment simpler and safer by blocking extra (variant) arteries that almost half of normal people have and utilizing collateral (detour) vessels inside the liver to assist in microsphere delivery. “After blocking these variant arteries, we were able to treat nearly 100 percent of tumors through the main hepatic artery”taking advantage of the networks of blood vessels within the liver,” reported Sze.

“By embolizing small, less important vessels to the tumors, one main arterial channel was created that could treat the entire area in a technically simple and practical way,” Salem explained. He also noted that these principles may be applicable to other embolization procedures, such as drug-eluting bead chemoembolization using microspheres that have been impregnated with a chemotherapy agent rather than radioactivity. “Based on this research, more people who are not good candidates for surgery will benefit in several ways,” he explained.
Be a part of Elets Collaborative Initiatives. Join Us for Upcoming Events and explore business opportunities. Like us on Facebook , connect with us on LinkedIn and follow us on Twitter , Instagram.