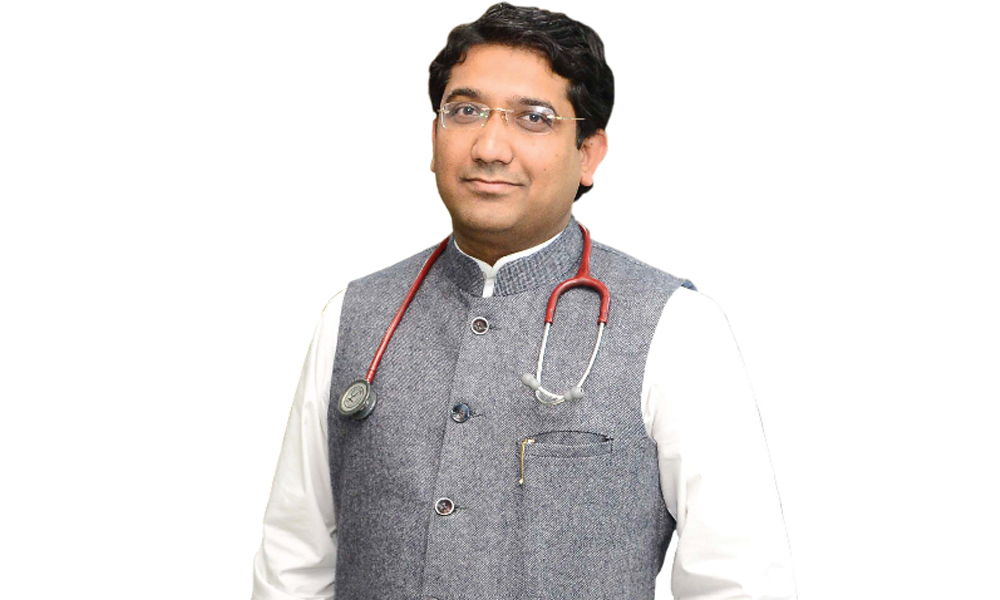
 Immunotherapy has emerged as a potent weapon in oncologists armoury to combat cancer, says Dr Sajjan Rajpurohit, a leading Medical Oncologist with over 10 years of experience in helping people revive the bodys magical immune system to fight the deadly disease, in an interview with Vivek Ratnakar of Elets News Network (ENN). Excerpts:
Immunotherapy has emerged as a potent weapon in oncologists armoury to combat cancer, says Dr Sajjan Rajpurohit, a leading Medical Oncologist with over 10 years of experience in helping people revive the bodys magical immune system to fight the deadly disease, in an interview with Vivek Ratnakar of Elets News Network (ENN). Excerpts:
Imagine a scene from the 1978 Hollywood flick Piranhas where a school of ferocious piranhas are hell bent on sucking out the very life out of a bather in South Americas Amazon River. Now, scale it down to millions of times to molecular level and imagine a host of viruses, bacteria and parasites attacking our cells to cause life-threatening diseases. But here is the catch. While the bather in Amazon may not be so lucky as to be able to defend himself from the deadly fish, our bodys magical shield, called immune system, straightaway swings into action to kill the potentially damaging foreign bodies.

References to our bodys immune system ” a collection of structures and processes within the body — are as old as the human civilisation itself.
Athenian historian and general Thucydides, who survived the Plague of Athens in 430 BC, points out in his History of the Peloponnesian War that people who had previously contracted the disease and recovered could help treat the sick without falling ill a second time.
There exists a huge body of work on immunity which was exploited by the likes of Louis Pasteur, Robert Koch, Paul Ehrlich and Elie Metchnikoff, the founder of cellular immunology, to make great advances in the field.

However despite all the strengths of the bodys immune system, when it comes to combating cancer, which in Latin means crab or creeping ulcer and was earlier applied to tumours because the swollen veins around them resembled the limbs of a crab, things start to change as cancer cells — being the altered self-cells — escape it and continue to grow uncontrollably.
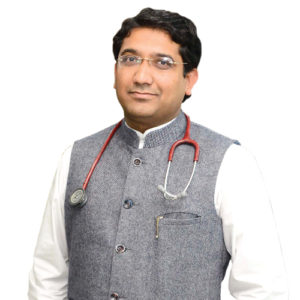 Tumour cells are unique in the sense that they are bodys own cells but the bodys check mechanism is unable to control them. So, when a person develops cancer, it means that his own body cells change into a type which grow abnormally, uninterrupted and use bodys own resources to drive their growth. It has a harmful effect on the body by sucking out all the energy towards their growth and not only they grow locally but also spread to other parts of the body and disrupt the other body functions, says Dr Sajjan Rajpurohit, a renowned specialist in medical oncology with a keen focus on immunotherapy and celluar therapy for cancer.
Tumour cells are unique in the sense that they are bodys own cells but the bodys check mechanism is unable to control them. So, when a person develops cancer, it means that his own body cells change into a type which grow abnormally, uninterrupted and use bodys own resources to drive their growth. It has a harmful effect on the body by sucking out all the energy towards their growth and not only they grow locally but also spread to other parts of the body and disrupt the other body functions, says Dr Sajjan Rajpurohit, a renowned specialist in medical oncology with a keen focus on immunotherapy and celluar therapy for cancer.
Our immunity fights against bacteria, viruses and fungi by recognising them as foreign bodies different from normal cells. But cancer cells mask themselves with normal cells to escape immunity. This phenomenon has been known for many years and it is also known that people with low immunity develop more cancers like people on steroids or post-transplant patients, he adds.
Efforts have been ongoing for many years to enhance immunity towards cancer, according to Dr Rajpurohit. But till now we have not been able to make a breakthrough. The specific immunity in the body is by T cells, which are the main source of direct killing of foreign body.
After over two decades of untiring efforts to understand how tumours escape the bodys immune system and how to use our own immunity to fight cancer cells, groundbreaking results are being seen in many small but landmark studies. The impact seems so promising that The Science magazine has labelled this approach as the Breakthrough of the Year 2013.
Dr Rajpurohit recalls a case that bears a testimony to how immunotherapy for cancer can be the next big thing in combating the disease.
In August 2015, a case of 56 years old gentleman, a chronic heavy smoker who had been smoking at least one to two packs of cigarettes for the last 30 years, was presented to me. He was having blood in the sputum, weight loss and cough for the last six weeks, and there was some degree of backache. He was referred to me by a chest physician who suspected a lesion in the x-ray.
Dr Rajpurohit uated him and got the PET-CT scan done, which showed there was a large lesion in the right lung and there were metastases in bones and the liver. He was confirmed to have lung cancer. We started giving him chemotherapy and after three cycles of chemotherapy, he started responding to the treatment. But after six cycles of chemotherapy, his condition worsened.
By that time a new class of drugs was introduced in the market, which might have been effective in such cases. So, I got his marker tested for immunotherapy and he was found to possess a strong positivity, indicating that he might get benefitted by immunotherapy.
Drugs were procured from overseas because at that time the drug was not available in India. Dr Rajpurohit started his treatment in February last year. After three doses of the drug, he showed significant improvement and after six doses of the drug he was almost like a healthy person. He regained his weight, his bone pain had disappeared and coughing seized. He is now enjoying a normal life, says Dr Rajpurohit, who has been trained in cancer treatment at Rajiv Gandhi Cancer Institute, Tata Memorial Hospital and MD Anderson Cancer Center Houston, Texas.
As a result of the clinical cancer research, more people are surviving cancer than ever before. According to Dr Rajpurohit, the current survival rate has double over the last two decades. Patients are being identified with cancer at an early stage leading to higher cure rates and patients with advanced stage (3rd and 4th) are leading healthier lives compared to before, he says.
The Global Evolution of Immunotherapy
The idea of using immunotherapy to treat cancer relies heavily on tweaking our immune systems potency to fight cancerous cells. But understanding how exactly they evade detection and ways to make them visible to the immune system is the subject of recent researches to make it work, Dr Rajpurohit points out.
As per the statistics, there are 14-15 lakh new cancer patients each year in India. In accordance with this fact, the focus should be on its prevention. We also need to make sure that the care we provide offers real value to our patients and we should put in an effort to improve the affordability and quality of medical care.
 The early steps were taken by cancer immunologist James Allison, now at the University of Texas MD Anderson Cancer Center in Houston, which is also the alma mater of Dr Rajpurohit.
The early steps were taken by cancer immunologist James Allison, now at the University of Texas MD Anderson Cancer Center in Houston, which is also the alma mater of Dr Rajpurohit.
In the late 1980s, French researchers who werent thinking about cancer at all identified a new protein receptor on the surface of T cells, called cytotoxic T-lymphocyte antigen 4 or CTLA-4. Allison found that CTLA-4 puts the brakes on T cells, and prevents them from launching all-out immune attacks. He wondered whether blocking the blocker, the CTLA-4 molecule, would set the immune system free to destroy cancer.
CTLA-4 was discovered in 1987. In 1996, Allison published a paper in the Science describing that antibodies against CTLA-4 erased tumors in mice. It took more than a decade to bring this approach from bench to bedside.
The Japanese biologists working on immune system discovered a molecule expressed in dying T cells, which they called programmed death 1, or PD-1.Oncologist Drew Pardoll at the Johns Hopkins University, thought of the approach of using own T cells against the cancer cells. He tied up with Medarex to test this antibody.
Last two years have seen more than a dozen of these potent T cell stimulating antiboidies entering large clinical trials with many getting breakthrough approval in cancers of lung, head and neck, colon, Iymphoma and Melanoma.
For years, Steven Rosenberg at the National Cancer Institute had harvested T cells that had migrated into tumors, expanded them in the lab, and reinfused them into patients, saving some with dire prognoses. The technique worked only when doctors could access tumour tissue, though, limiting its application. In 2010, Rosenberg published encouraging results from so-called chimeric antigen receptor therapy, or CAR therapy, a personalised treatment that involved genetically modifying a patients T cells to make them target tumour cells. Carl June and his team at the University of Pennsylvania, reported eye-catching responses to CAR therapy: patients with pounds of leukemia that melted away. At a meeting in New Orleans, Junes team and researchers at Memorial Sloan-Kettering Cancer Center in New York reported that the T-cell therapy in their studies put 45 of 75 adults and children with leukemia into complete remission, although some later relapsed.
Indian Scenario
As per the statistics, there are 14-15 lakh new cancer patients each year in India. In accordance with this fact, the focus should be on its prevention. We also need to make sure that the care we provide offers real value to our patients and we should put in an effort to improve the affordability and quality of medical care. The National Cancer Control Programme should be change-driven in terms of attitude and practice with regards to cancer detection and management, says Dr Rajpurohit.
| FRESH APPROACHES IN IMMUNOTHERAPY |
|
Adoptive T Cell Therapy (ACT) TIL Therapy Chimeric Antigen Receptors (CARs) Anti-tumour Antibodies |
Despite numerous advances in medicine, according to a 1999 report on cancer occurrence in India it was estimated that more than 50 per cent of the total number of cancer cases were reported among women. The crude incidence of cancer in India is approximately 100 per 100,000 people. Recent epidemiological studies done at the National Cancer Registry programme in India report that cancer burden in the country is 2.5 to 3 million.
Corrective steps like cancer screening programme should become a part of health awareness camps. There is a need to create awareness among physicians to facilitate early referral to cancer centers for improved outcomes, adds Dr Rajpurohit.
All the treatments are available in India. There is no need to go to any foreign destination, according to him.
New Immunotherapy Approaches
Although the common treatment modalities, such as surgery and/or chemo and radiotherapies, play major roles in bringing down the mortality and morbidity to a significant extent, complete cure is still uncertain and the prognosis varies depending upon the stage and the type of the disease.
Even when patients experience tumour regression immediately after therapy, recurrence or metastasis (spreading to other parts of the body) can occur later.
Immunotherapies have the potential to be used to fight cancer by either applying an external stimulus to the immune system to make it act more smarter, or by providing the immune system with man-made or naturally-derived tumor specific proteins made outside of the body so that the immune system can recognise the tumour as a foreign entity and destroy it.
Efforts have been ongoing for many years to enhance immunity against cancer but till now we have not been able to make a breakthrough. The main immunity in the body is through T cells. They are the direct source of killing the foreign body. How do these tumour cells interact with them? They have their expression of some molecule on the surface, which is known as PDL1 “ Programmed Death Ligand 1. They programme the death of T cell. We have developed antibodies against PD or PDL1 which kills the T cells. We have made antibodies which blocks the interaction of T cells with PDL and PDL1. In this way, T cells dont die. This has happened recently. This is our key achievement. They are called PDL1 antibody. They make the T cell active, says Dr Rajpurohit.
Scientists have also been able to genetically engineer T cells. We take T cells out of the body and insert new receptors in them, which activates the T cells against the tumour cells. These are called CAR T cells. It is a breakthrough in blood cancer. Children who were left untreated are getting treated due to this new technology. It is a big success. The only challenge is that we are not able to mass produce this technology on bigger scale, adds the leading oncologist, as he briefs about the new class of drugs which is highly effective in fighting cancer.
Many of these new classes of drugs are available in India. The ones which are not available in the country can easily be procured, according to Dr Rajpurohit.
Cost is the only limitation for these new class of drugs. But realizing their benefits, the government too is proactively looking to bring the cost down. In the next five years, their cost will definitely come down, he says.
Be a part of Elets Collaborative Initiatives. Join Us for Upcoming Events and explore business opportunities. Like us on Facebook , connect with us on LinkedIn and follow us on Twitter , Instagram.












