LIS can ensure quicker availability of test results and analysis in ICUs, operating rooms or emergency room settings. The faster turnaround times by reducing the time to report can save invaluable patient lives. LIS can be integrated with point of care diagnostic devices at these locations for information management. The value of providing detailed results to clinicians in real time cannot be undermined.
A majority of the initiatives advocating the use of information technology in hospitals or clinical practices, focus on electronic medical record systems. While the advantages of EMR systems have been substantially proven, an often-overlooked aspect of healthcare delivery automation is the use of information technology in clinical laboratories.

Imaging services are leading the technology adoption curve in healthcare while the laboratory information systems lag quite behind. Imaging tools are closely integrated with computerized systems for display and communication of data, so there is relatively no process disruption by the introduction of radiology information systems. Similarly, the need to track inventory has propelled pharmacies as one of the drivers to adopt information systems, which are now being linked to EMRs for e-Prescriptions. However, laboratories have been using paper-based systems. Here the automation has been patchy and the lack of widely accepted standards and protocols for data communication has impeded the concerted effort to make the laboratory systems talk.
Laboratory investigations consume a small proportion of the healthcare budget, but influences a great percentage of clinical decisions. In a study, it was indicated that the laboratory tests comprised 3-5 percent of the hospital’s budget, but influenced about 60-70 percent of the decisions about admitting patients, ordering medications or discharges. Both ‘Laboratory Information Management Systems (LIMS)’ and ‘Laboratory Information Systems (LIS)’ refer to the software systems used in laboratories, however, in a hospital setting, LIS is more prent.
Laboratory Information System
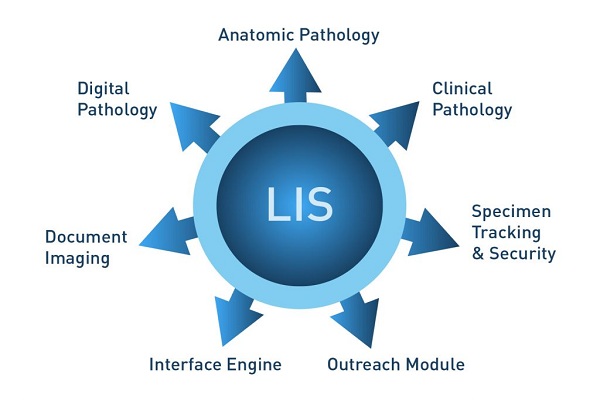
Laboratory Information System is a generic term used to denote the computer systems in a clinical or research laboratory. LIS has multiple modules for data collection, tracking, analyzing, reporting or delivery of results. The data can be related to patients, lab employees, samples, results, instruments, consumables or reagents, etc. LIS can also be used for workflow management, accounts and control of instruments if integrated with the system. The LIS is interfaced with Electronic Medical Record (EMR) or Hospital Information System (HIS) for exchange of data, and faster access of laboratory results at the patients’ bedside. LIS can support various sub-specialties of a pathology laboratory including hematology, chemistry, immunology, blood bank, surgical pathology, anatomical pathology, flow cytometry and microbiology. The inputs into a LIS are a uniquely identifiable physician order and a matching patient sample. These are then matched with the patient record and the order is processed. The outcome of the test is then manually or electronically added to the patient record for access by the physician.

LIS can generate bar-codes or a unique identifier for the samples. This helps in easier, faster and error free tracking of samples. If the testing instrument is automated, which is in most cases, samples are uploaded in batches and the analyzing instruments match the results and relay them directly to the LIS system. In case of manual systems, a technician matches the results with the samples and the patient, and enters the data into the system. These are either printed on the lab report or sent to the hospital medical record system.
LIS also stores the demographic information of the patients, tests orders, and results for retri. Furthermore, LIS collects the data from multiple testing departments, instruments or locations into a single report and database. A very useful purpose of LIS is to support the ordering clinician with various options of tests that he or she could choose from with indicators for each patient. These systems could be standalone or be operated by a clinical pathologist for advance decision support. In some hospitals, such systems have been piloted and the physicians are increasingly turning to expert advice for laboratory investigation selection and also interpretation advise to increase the quality of care, reduce medical errors and decrease the cost of care.
Standards
In order to ensure interoperability and seamless exchange of clinical information, global standards have emerged, which enable the adoption of LIS technology without worrying about interfaces. SNOMED (Systematized Nomenclature of Medicine Clinical Terminology) is the industry standard for representation of medical terminology in electronic systems. It harmonizes the collection, encoding, storage, sharing and transmission of clinical data, including disease nomenclature, procedures, pathogens, pharmaceuticals, etc. The standardization helps healthcare providers working across countries, healthcare systems and dialects to effectively communicate, report and make transactions, thereby facilitating in seamless and accurate exchange and aggregation of laboratory results.
Using Health Level 7 (HL7) standards, guidelines, and methodologies, LIS are able to exchange data with electronic health records, ensuring interoperability across various healthcare networks. HL7 is the standard for interfacing clinical data in Health Information Systems.
The Area Committee on Automation and Informatics of the Clinical and Laboratory Standards Institute (CLSI) identifies, manages and coordinates the development of standards and guidelines for the design and integration of automated clinical laboratory. Logical Observation Identifiers Names and Codes (LOINC) is the standard for identifying laboratory or clinical observations, test names and outcomes in transactions between hospitals, laboratories, laboratory testing instruments and public health authorities.
LISt of Benefits
Laboratory Information Systems provide a number of benefits, which undeniably provide a great incentive towards their adoption. Some of the benefits that healthcare organizations can derive from such systems are elucidated here.
LIS can ensure quicker availability of test results and analysis in ICUs, operating rooms or emergency room settings. The faster turnaround times by reducing the time to report can save invaluable patient lives. LIS can be integrated with point of care diagnostic devices at these locations for information management. The value of providing detailed results to clinicians in real time cannot be undermined. In a study conducted at Massachusetts General Hospital, the clinicians’ improved accuracy in 70-80 percent of the cases using expert opinions of pathologists were facilitated by LIS. The concerned pathologist used a LIS with clinical decision support to provide narrative interpretation with every lab result to cohort of clinicians.
Disease surveillance for earlier detection of epidemics is another important benefit. LIS systems can be connected with a central monitoring system, which picks up subtle changes in trends. Such a system is being set up under the World Bank funded Integrated Disease Surveillance Project in India. LIS can provide surveillance data to public health agencies, using the accepted standards, and these data could be about reportable disease, infections, tumour registries, etc.
 LIS can also facilitate evidence-based medicine. The systems can be used for trend analysis, tracking of disease profiles and conducting research studies. Laboratories generate a lot of data, running into millions of test outcomes everyday. These data can be matched with the appropriate clinical records to determine outcomes, which could dynamically influence the treatment plan. In a study, about 25 percent of primary care physicians found the expectations of care beyond the scope of their knowledge.. The physicians will be well served with a LIS which helps to provide interpretations to ordering physicians that are specific to patients’ needs and conditions.
LIS can also facilitate evidence-based medicine. The systems can be used for trend analysis, tracking of disease profiles and conducting research studies. Laboratories generate a lot of data, running into millions of test outcomes everyday. These data can be matched with the appropriate clinical records to determine outcomes, which could dynamically influence the treatment plan. In a study, about 25 percent of primary care physicians found the expectations of care beyond the scope of their knowledge.. The physicians will be well served with a LIS which helps to provide interpretations to ordering physicians that are specific to patients’ needs and conditions.
LIS also helps to ensure better quality of care by providing comprehensive interpretation of tests; decision support during ordering and earlier detection of adverse events. Increasingly, the general practitioners feel that the clinical information is growing too fast for them to keep track of. So a LIS with decision support can be usefully integrated with the Computerized Physician Order Entry System (CPOE). Just as CPOE systems have been very successful in the selection of appropriate medications, use of similar systems for laboratory test selection will improve the patient safety and quality of care. In another study, a decision support system was put in place to assist the physician with ordering tests. The study indicated that the physicians who used this system, ordered lesser number of tests, leading to reduced sample collection and costs. LIS can lead to inventory management without the use of bar-code systems or radio frequency IDs. Automation in the laboratories will provide the same benefits as any retail or service industry.
Another potential benefit is the error reduction in labelling and interpreting by automating the process of sample collection, testing and reporting. Using unique identifiers for physician orders, patients and samples, potentially dangerous mistakes can be avoided. Studies have shown improvement in patient safety with the use of information technology tools. There can be improved communication between departments by connecting LIS with the Hospital Information System, which can result in cost savings and increase in productivity. The laboratory diagnostic tools are becoming complex. Emergence of molecular diagnostics will further increase the dependence on information technologies for interpretation and management of test results. Increase in utilization and testing options frequently puts uncertainty among the ordering clinicians choice of investigations, resulting in inappropriate ordering in some cases.
Regulatory compliance by incorporating checks and alerts in the laboratory management workflow is another possible benefit. Laboratory requirements can be programmed into the systems so as to generate alerts for warnings or for deviations from protocols. These are of immense help in QA activities and in ensuring compliance with government and regulatory compliance. Easier and quicker billing by integration with hospital accounting systems can prevent much undue hassles.
Current issues
However, notwithstanding the potential benefits of LIS, Laboratory Information Systems have to cover some ground before they become ubiquitous. Some of the issues in LIS are around:
Integration with EMR systems of the hospitals. Even though standards for exchange of patient information exist, sometimes it becomes a challenge to integrate with legacy EMR systems.
Paucity of intervention free, intelligent and reliable decision support to the ordering physicians. Due to the complexity of clinical practice, a same test may not be ordered for two different patients, maybe because the family history is different or patients can’t afford it. The LIS have not become sophisticated enough to consider all practical permutations.
General poor state of automation of clinical laboratories resulting in barrier to adoption. In a resource-starved setting, introduction of LIS can be considered an overkill.
Appropriate training of lab techs in information technology tools is also the need of the hour.
HIPAA and privacy issues around sample management needs a concern. Electronic information has the potential of abuse, but with wider adoption of EMR systems, these concerns have subsided.
Conclusion
Laboratory Information Systems have come a long way, but are poised for even greater growth as complex medical investigations become more pervasive. With increasing use of molecular diagnostics, biomarker-driven testing tools and genomic technology in clinical practice, the LIS will become indispensable. A lot of work still needs to be done for algorithm development and decision analysis to fully support the physicians in the selection and interpretation of tests, but the ongoing developments in evidence-based practice of medicine have been very encouraging.
The problem so far has been the complexity of such decisions. Currently, there is no widely acceptable algorithm-driven test selection and interpretation software. However, in the future, with the adoption of sophisticated biomarker-based diagnostic tools, data warehousing studies on patient registries and use of search engine technologies on large patient databases, such applications are possible.
References
1.Forsman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem 1996;42:813-816
2.Laposata M. Patient-specific narrative interpretations of complex clinical laboratory uations: who is competent to provide them?. Clin Chem 2004;50:471�472
3.Health data standards: The Players. (https://faculty.washington.edu/ocarroll/infrmatc/database/data/players.htm. Accessed July 15, 2007)
4.Clinical and Laboratory Standards Institute, Area Committee on Automation and Informatics (https://www.nccls.org/source/custom/comm_aut.cfm?Section=Area_Committee_on_Automation_and_Informatics. Accessed July 15, 2007)
5.Laposata ME, Laposata M, Van Cott EM, Buchner DS, Kashalo MS, Dighe AS. Physician survey of a laboratory medicine interpretive service and uation of the influence of interpretations on laboratory test ordering. Arch Pathol Lab Med. 2004;128:1424-1427
6.The World Bank, Integrated Disease Surveillance Project. (https://web.worldbank.org/external/projects/main?pagePK=104231&piPK=73230&theSitePK=40941&menuPK=228424&Projectid=P073651. Accessed July 15, 2007)
7.St. Peter FR, Reed MC, Kemper P, Blumenthal D. Changes in the scope of care provided by primary care physicians. N Engl J Med 1999;341:1980-1985
8.Teich JM, Merchia PR, Schmiz JL, et al. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741-2747
9.Smith BJ, McNeely MDD. The influence of an expert system for test ordering and interpretation on laboratory investigations. Clin Chem. 1999;45(8 pt 1):1168-1175
10.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med 2003;348:2526�2534
11.Berwick DM. A primer on leading the improvement of systems. BMJ 1996;312:619�622
12.Green ML, Ciampi MA, Ellis PJ. Residents’ medical information needs in clinic: are they being met?. Am J Med 2000;109:218�223
13.Dighe AS, Soderberg BL, Laposata M. Narrative interpretations for clinical laboratory uations: an overview. Am J Clin Pathol 2001;116 (suppl). :S123�S128
Be a part of Elets Collaborative Initiatives. Join Us for Upcoming Events and explore business opportunities. Like us on Facebook , connect with us on LinkedIn and follow us on Twitter , Instagram.












