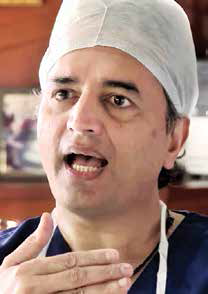
Dr Devi Shetty, Cardiac Surgeon,
Narayana Hrudayalaya,
Bangalore
Treating over 26 lakh beneficiaries – government employees, pensioners and their families, of them 400,000 from Delhi and NCR currently covered under Central Government Health Scheme (CGHS), the major hospitals around the country finally raise their concerns about the rising pending bills and rates uniformity.
By Ekta Srivastava, ENN

CGHS is the mother of all health schemes. For Universal Health Coverage to protect weaker sections of the society, it is important that remuneration and timely payment for CGHS schemes are standardized. This will help charitable and private hospitals to extend their services to all the government sponsored health schemes. It is important for CGHS scheme to work with the network hospitals and address their grievances,said, Dr Devi Shetty cardiac surgeon, Narayana Hrudayalaya, Bangalore
Members of Association of Healthcare Providers India (AHPI) along with key private healthcare providers in India recently express their concerns on CGHS. According to them, most of the charitable and private hospitals, which are empanelled under CGHS to treat Central Government employees and pensioners, are not being reimbursed within reasonable time for the healthcare services offered. Moreover, the tariff for procedures arrived by CGHS is very low. As a result, the services to CGHS beneficiaries are not financially viable for private and charitable hospitals.
CGHS has recognized a number of charitable and private hospitals and diagnostic centers across the country and so its beneficiaries can access specialty and super-specialty healthcare facilities in these empanelled hospitals. The package rates are fixed by CGHS for different procedures and medical treatments. The empanelled private hospitals and diagnostic centers are required to provide cashless treatment to pensioners and their dependants holding valid CGHS card and referral from CGHS authorities. They are also expected to extend services to the pensioners and their dependants in case of medical emergency on showing of only the CGHS card.
Hospitals import expensive diagnostic and medical equipments paying high import duties. In some cases it takes 7 to 10 years to recover the cost of equipment and consumables. With steep increase in foreign exchange rate in the last few years and funds crunch due to non-payment from CGHS, the hospitals are getting into huge debts, incurring heavy interests from the banks while funding the government schemes.
The hospitals have been in discussion with the Director General of CGHS on the issues since May 2013. The issues have not been addressed or resolved till now.

| The Associations of Hospitals across the country request for: |
| Scientific and realistic revision of tariff for procedures Automatic annual revision of tariff based on Consumer Price Index On time payment Clearance of pending bills Refund of 10% discount illegally deducted by UTI (to all hospitals for payment after 10 days) and stoppage of processing fee being charged by UTI 24 hr grievance cell Regular involvement with stake holders in decision making Refund of unauthorized deductions from running bills |
AHPI Concerns
The AHPI, which claims to represent around 10,000 private and charitable hospitals across the country, also asked the government to look into revision of rates for various procedures, anomalies in payment structure and refund of unauthorised deductions from running bills.
The AHPI comprises the biggest private hospitals in India including the Apollo Group of Hospitals, Medanta, Fortis Healthcare, Max Healthcare, Sir Ganga Ram, PD Hinduja, Lilavati and Narayana Health.
The hospitals believe that this move will spur the system to correct the prevailing anomalies and establish better working arrangement benefiting all stakeholders, APHI director General Girdhar J Gyani told.
With steep increase in foreign exchange rate and funds crunch due to non-payment from CGHS, the hospitals are getting into huge debts, incurring heavy interests from banks while funding the government schemes, he added.

Different Tariffs
This scheme has been considered as a benchmark or framework for several healthcare schemes in India. Hospitals offer services to the scheme holder patients at a fee structure lesser than the normal rates and in credit. However, there is no uniformity in the rates in any hospitals, for example MRI Orbits Code 367. Charges in Bangalore is `600 and in Chennai and Hyderabad it is ` 5000
The tariff for procedures arrived by CGHS is very low. As a result, the services to CGHS beneficiaries are not financially viable for private and charitable hospitals, Gyani said.
Dr Giridhar Gyani,
APHI director General
Since 2002, there has been no revision in the CGHS tariffs while in certain procedures, the rates were arbitrarily reduced. The members unanimously decided to demand a scientific costing analysis so that the government comes up with revised tariffs for all the service providers.
Some of the tariffs are way too low. For instance, a mitral valve replacement under the Yashaswini rural health care scheme (Karnataka government) costs `80,000 but under CGHS, it costs `55,000. CGHS beneficiaries are not poor. More than the issue of rates per se, the payments as per the scheme are delayed. To make matters worse, there are many deductions as well, said Dr Shetty. We need to survive first to serve others, he added.
Pending dues
Private hospitals include the countrys biggest set-ups like B L Kapoor, Medanta Medicity and Dharamshila Cancer Hospital in Delhi/NCR, Baptist Hospital in Bangalore and Ruby Hall Clinic in Pune, which have the pending bills tune up to `125 crore to be cleared.
The private and charitable hospitals have come together to convey that if these issues are not resolved immediately, these hospitals will be constrained to withdraw the cashless facility to CGHS beneficiaries with effect from 15th January 2014 in Delhi, Andhra Pradesh and Karnataka followeped by other states across the country. However, the CGHS beneficiaries can continue to avail treatment against payment at CGHS tariff, reported by AHPI. The hospitals believe that this move will spur the system to correct the prevailing anomalies and establish better working arrangement benefiting all stake holders.
They promised prompt payment recently but it has not materialised so far. If the government does not resolve the issue, hospitals across India will have to unanimously decide to stop the cashless treatment starting next year, said Dr B Bhaskar Rao, President, ASHA. The CGHS tariffs were fixed in a haphazard manner, he said. While beneficiaries of the CGHS have alleged that CGHS-empanelled private hospitals are treating them indifferently and giving them a stepmotherly treatment.
Be a part of Elets Collaborative Initiatives. Join Us for Upcoming Events and explore business opportunities. Like us on Facebook , connect with us on LinkedIn and follow us on Twitter , Instagram.
"Exciting news! Elets technomedia is now on WhatsApp Channels Subscribe today by clicking the link and stay updated with the latest insights!" Click here!
















